What Is IBS? Causes, Symptoms & Treatment Options Explained
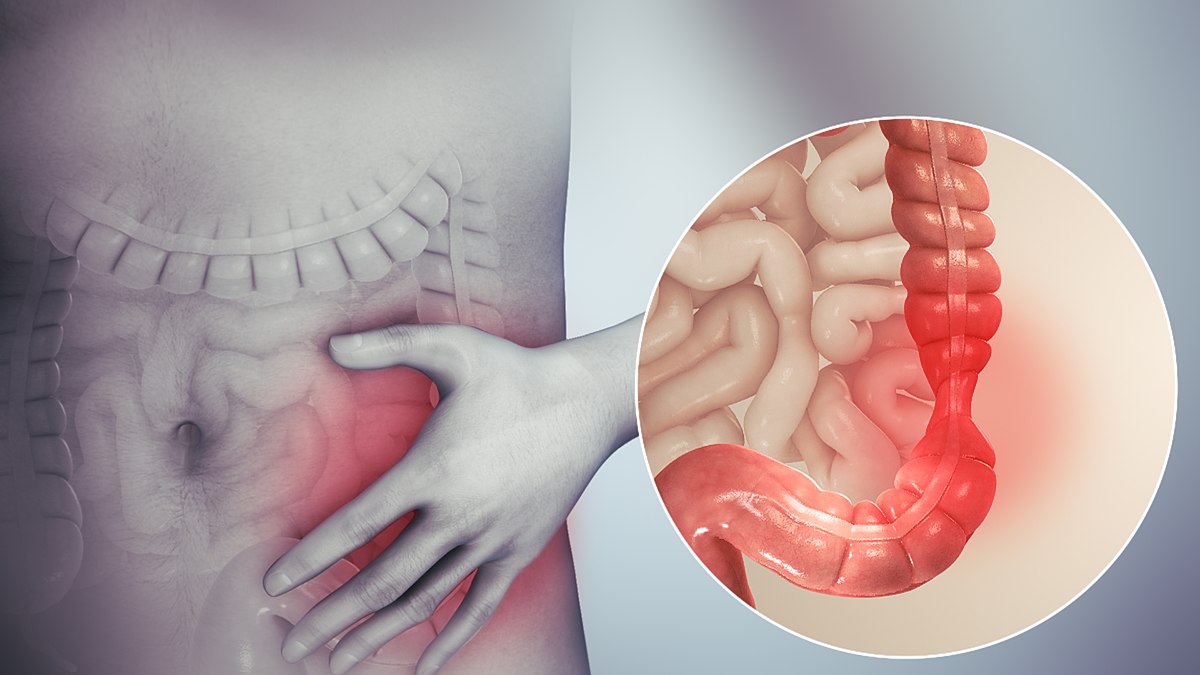
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal condition that affects the large intestine. It is characterized by recurring abdominal discomfort and changes in bowel habits, including diarrhea, constipation, or a combination of both. While not life-threatening, IBS can significantly impact the quality of life, requiring ongoing management to alleviate symptoms and maintain digestive health. If you’re wondering what is IBS, understanding its symptoms, causes, and management strategies is essential.
Understanding IBS: Symptoms and Types
1. Symptoms of IBS:
- Abdominal pain and cramping: Often relieved after bowel movements.
- Bloating and gas: A frequent complaint among individuals with IBS.
- Altered bowel habits:
- IBS-D: Predominantly diarrhea.
- IBS-C: Predominantly constipation.
- IBS-M: A mix of both diarrhea and constipation.
- Mucus in stool: Common in some cases.
- Fatigue and difficulty sleeping: These are often associated symptoms, especially during flare-ups.
2. Types of IBS:
- IBS with Constipation (IBS-C): Hard, lumpy stools with infrequent bowel movements.
- IBS with Diarrhea (IBS-D): Loose, watery stools with frequent urgency.
- Mixed IBS (IBS-M): Alternating between diarrhea and constipation.
Causes of IBS
The exact cause of IBS remains unclear, but several factors are believed to contribute to its development:
- Gut-brain axis dysfunction: Miscommunication between the brain and gut can alter intestinal movements and sensitivity.
- Abnormal gut motility: Disrupted movement in the digestive tract leads to irregular bowel habits.
- Microbiome imbalance: Changes in gut bacteria may contribute to symptoms.
- Stress and mental health: Psychological factors like anxiety and depression often exacerbate IBS.
- Food sensitivities: Certain foods can trigger symptoms, such as gluten, dairy, or high-FODMAP items.
Diagnosing IBS
There is no definitive test for IBS. Diagnosis is typically based on:
- Rome IV Criteria: Identifying abdominal pain associated with bowel movement changes for at least six months.
- Exclusion of other conditions: Tests to rule out inflammatory bowel disease (IBD), celiac disease, or infections.
Managing IBS: Lifestyle Changes and Treatment
1. Dietary Adjustments:
- Low-FODMAP diet: Reducing fermentable sugars found in foods like garlic, onions, and certain fruits.
- Fiber intake: Increasing soluble fiber can help with IBS-C, while insoluble fiber may worsen symptoms for some.
- Identifying triggers: Keeping a food diary to pinpoint problematic foods.
2. Stress Management:
- Mindfulness and relaxation techniques: Yoga, meditation, or deep breathing exercises.
- Therapy: Cognitive Behavioral Therapy (CBT) has proven effective for some individuals.
3. Medications:
- Antispasmodics: Relieve abdominal cramps.
- Laxatives or antidiarrheals: Address specific bowel issues.
- Probiotics: May help restore gut flora balance.
4. Regular Exercise: Promotes gut motility and reduces stress.
When to Seek Medical Help
Consult a healthcare provider if you experience:
- Unexplained weight loss.
- Rectal bleeding.
- Persistent pain that doesn’t improve with management.
- Signs of nutrient deficiencies or extreme fatigue.
Living with IBS
While IBS has no cure, a combination of lifestyle changes, dietary adjustments, and stress management can help individuals lead a comfortable life. Support groups and resources are also valuable for coping with the condition.
For more resources on maintaining digestive health, check out TuberBuddy for articles on wellness and diet.